This Device is Small Enough to Be Injected into the Human Body
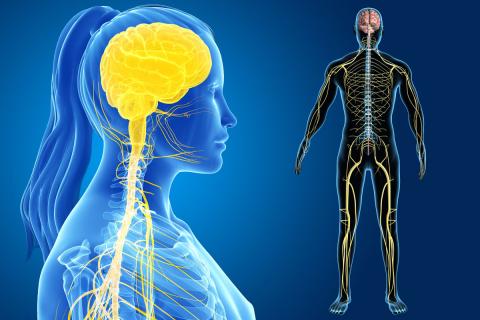
CAMBRIDGE, MA—Epilepsy, incontinence, Parkinson’s disease and many other health conditions all have one thing in common: the human nervous system. There are nearly 46 miles of nerves in an adult’s body, and the newest frontier of medicine is to explore ways to stimulate and modulate neurons so that one day patients will gain the ability to control their symptoms. But there are engineering challenges to doing so.
“Building a device small enough to be injected into the human body that can operate wirelessly and does not require surgery every time it needs a new battery is a real challenge,” said Daniel Freeman, a senior research engineer and electrophysiologist at Draper.
In addressing this problem, Freeman and a team of engineers developed a proof-of-concept for a sub-millimeter, inductively-powered neural stimulator that reduces the number of electronic components without sacrificing performance. In November, they published a paper that described this new kind of wireless neural stimulator that is small enough to clip directly onto a nerve and deliver enough current to activate nerves in the body. The device is 2.5 millimeters long with wires 0.5 millimeters in diameter, making it five times smaller than other radio-powered wireless stimulators. It consists of a coil to receive power, a capacitor to tune the resonant frequency of the receiver and a diode to rectify the radio-frequency signal to produce neural stimulation.
An important advance in making the device as small as possible was to encapsulate it in epoxy approved by the FDA for use in medical implants, rather than titanium or ceramic, which tends to make such devices bulky. Stimulators on this size and scale would allow the electronics and antenna to be entirely integrated into a cuff for a peripheral nerve. The project is an important one for Draper and it is part of a larger and growing neurotechnology portfolio that includes next-generation devices for restoration of sensation for amputees.
“We believe the device could be used in any number of applications in the peripheral nervous system,” said Freeman. “One exciting application for this device is in the treatment of chronic pain as an alternative to opiates. The patient can apply the stimulation intermittently or continuously, depending on the need. The same approach could apply to urinary incontinence, inflammatory conditions or even high blood pressure.”
Bioelectronic medicine, otherwise known as electroceuticals or neuromodulation, may be the fastest-growing alternative to drugs. It has attracted more than $1 billion in investment in the past three years. Draper is engaged in the fundamental engineering and applied research underlying this emerging medical field and anticipates a day when the devices won’t just stimulate or modulate the nervous system but will turn individual neurons on and off to prevent disease.
The proof of concept for the implant was funded by Draper and accomplished in animal studies by Draper in collaboration with a team of electrophysiologists and neuroscientists at the University of Texas, led by Romero-Ortega and Stuart Cogan. The study demonstrated that the device was capable of exciting neurons in the sciatic nerve. Early animal studies are designed to evaluate the implants’ ability to reduce symptoms of disease and thus improve quality of life in humans.
Released December 8, 2017