Draper Brings Scalability to CAR T-Cell Bioprocessing
CAMBRIDGE, MA—A pioneering new kind of cancer therapy that uses genetically engineered cells from a patient’s immune system has a very bright future following studies that show 83 percent of patients in clinical trials had their cancer go into remission. A U.S. Food and Drug Administration panel agreed and unanimously endorsed the treatment, called tisagenlecleucel, for FDA approval. However, the FDA did note “a major consideration for manufacturing tisagenlecleucel is the establishment of a well-controlled manufacturing process that can consistently produce high-quality CAR T cells that are safe, pure, and potent.”
The new treatment uses a technology known as CAR T-cell immunotherapy. CAR T-cell therapy works by genetically modifying the patient’s own T cells so that they can recognize and kill cancer cells without damaging normal cells. That’s why some scientists refer to this treatment as a “living drug.”
“CAR T-cells are a promising therapy, but the current state of biomanufacturing is very complex, expensive and time-consuming, often requiring multiple rooms, highly skilled technicians and many instruments,” said Tara S. Clark, vice president of commercial programs at Draper. “What’s needed is a bioprocessing platform that can help cell therapy developers bring their therapies to market more quickly, safely and affordably.”
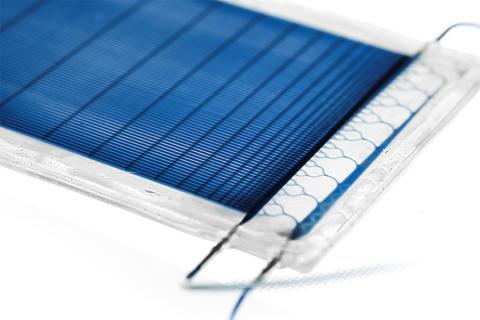
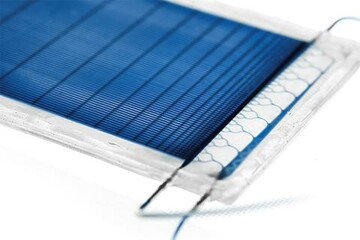
Draper has addressed this challenge by working to develop microfluidic platforms that will perform key steps of the CAR T-cell manufacturing process, as well as processes for other types of cell therapies. Draper’s innovations include a technique known as acoustophoresis for separating and enriching the immune system cell population that includes T cells using sound energy, as well as a platform for accelerating the process for transferring genetic material into T cells from the current one-to-three days to less than a day.
The goal of Draper’s microfluidic technologies is to create improvements in the cell therapy manufacturing process by combining fluidic control, precision and the ability to scale to higher throughput systems for easy integration with existing manufacturing equipment. The anticipated result will be a lower-cost, high-quality therapy that can be produced more quickly than is possible with current methods.
“Companies are trying to break through the bioprocessing bottleneck so they can scale up without losing quality,” said David O'Dowd, associate director of biomedical solutions at Draper. “As the cell therapy community moves closer to achieving the goal of a closed, end-to-end system that automates cell therapy bioprocessing—and delivers downstream benefits such as standardizing processes and minimizing human error and the risk of contamination—Draper will continue to deliver solutions that matter.”
Released July 19, 2017