Mapping the Brain to Address Mental Illness
CAMBRIDGE, MA – As many as 1 in 5 Americans suffers from a diagnosable mental disorder in any given year. Mental illness is the leading cause of disability worldwide, but traditional treatment options, including psychotherapy and medication, are no guarantee of relief from symptoms that hinder the normal activities of everyday life. Neuroscience suggests that mental disorders arise from abnormal brain circuits, and that traditional therapies may not target these underlying neural dysfunctions.
Deep Brain Stimulation (DBS), where precisely directed pulses of electrical current stimulate dysfunctional brain circuits to alter neural activity, is emerging as a viable alternative for the one in five patients who feel no relief from medication and psychotherapy.
In early tests, DBS showed promise for treating treatment-resistant depression and obsessive compulsive disorder (OCD). In clinical trials, however, those results could not be replicated. The poor outcomes could be explained by the open-loop nature of the implanted device, which means that stimulation was delivered not based on measured input, and without regard to when, and the degree to which, brain activity becomes dysfunctional. Because mental disorders are dynamic, meaning symptoms and neural dysfunction wax and wane over time, new research suggests that it is important to control stimulation based on when neural activity becomes dysfunctional.
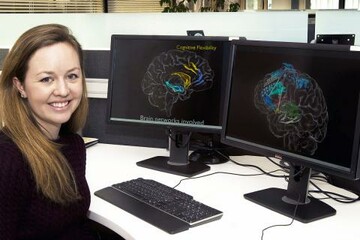
“Harnessing the full potential of DBS for the treatment of mental illness will require an adaptive, closed loop approach backed by quantitative measures of neural activity that signals when to turn stimulation on and off,” said Nicole Provenza, a Brown University graduate student, Draper Fellow and a member of a research team at Draper that is studying DBS.
Provenza is developing algorithms to accurately detect biomarkers of neural dysfunction. She is part of a team at Draper working towards a closed loop control system that promises to one day enable DBS treatment of neuropsychiatric disorders, including substance abuse, depression, bipolar disorder, attention deficit disorder, anxiety, post-traumatic stress disorder (PTSD) and traumatic brain injury (TBI). Provenza hopes her research on identifying and understanding the dysfunctional brain’s neural activity related to mental illness will enable the development of a long-term, durable brain implant—the equivalent of a pacemaker for the effective treatment of intractable mental illness.
Released May 24, 2017