Safer Treatment for Patients with Age-Related Vision Loss
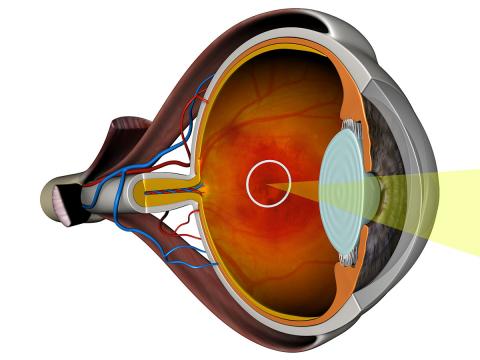
CAMBRIDGE, MA – Approximately 15 million people over 60 years old in the United States suffer from vision loss due to age-related macular degeneration (AMD). Identifying the small subset of 10-15 percent of those patients who are experiencing Wet AMD, which involves fluid accumulating in the retina that can cause irreversible damage and blindness, is a difficult challenge. Clinicians today study imagery of the eye to identify characteristic structures and changes in the retinal layers to diagnose Wet AMD and compare images taken over time to assess response to treatment – a subjective method. Clinicians lack objective criteria and measurements to help determine whether a patient would benefit from invasive options to slow Wet AMD. Those treatments, which include delivering drugs through an injection into the eye, often save a patient’s vision, but risk side effects including accelerating vision loss.
Draper is addressing this challenge with an automated diagnostic capability that analyzes retinal imagery. Initial studies of Draper’s solution using a set of imagery taken as part of patients’ initial evaluations and after treatments have correctly identified patients who will respond to Wet AMD therapies in more than 85 percent of cases.
“You may still need to give a patient an injection, but you will know in advance that they will benefit from the treatment,” said David O’Dowd, Draper’s associate director of Biomedical Solutions. “This prognostic capability can reduce harmful side effects, as well as medical expenses, from unnecessary treatment.”
Draper’s approach combines the company’s biomedical expertise with its growing portfolio of tools in big data analytics. This capability uses an algorithm to extract features in Optical Coherence Tomography (OCT) imagery, and compares them to a bank of imagery from patients whose treatment history and response to therapy is known from past experience. Clinicians then can consider a recommendation from the algorithm as to whether the patient is likely to respond positively to available Wet AMD treatments.
Initial results from this project were presented recently during the Association for Research in Vision and Ophthalmology (ARVO) conference in Seattle.
Next steps for the research include applying the algorithm to larger data sets to confirm its effectiveness and selecting a standard set of features for use in classifying Wet AMD patients.
“Additional data on more subjects would help us build a clearer understanding of the disease’s progression and provide a stronger foundation for validating our methods,” said John Irvine, Draper’s chief data scientist. “In addition to simply increasing the number of observations, we would also like to have data from patients at differing levels of severity and images collected by a variety of standard devices. All of these things will help us to develop and validate more robust and reliable methods.”
The solution would require clinical trials, which would not be handled by Draper, and could be ready within three years.
Work thus far has focused on analyzing OCT imagery in retinal diseases, but the same algorithm could be applied to imagery generated by CT scan, MRI, and ultrasound for other disease states like Alzheimer’s and non-Hodgkin’s lymphoma, O’Dowd said.
Released May 25, 2016