Stopping Killer Infections
CAMBRIDGE, MA – Patients with compromised immune systems, which can include those undergoing chemotherapy and organ transplants, risk death if they contract invasive aspergillosis, a fungal pneumonia with nonspecific symptoms. While invasive aspergillosis is a rare condition, it is on the rise due to factors including the increasing number of solid organ and stem cell transplant recipients. The mortality rate for patients with vulnerable immune systems is up to 58 percent, primarily due to delays in diagnosis. Existing tests are slow to yield results, often incorrect, and sometimes require invasive measures, such as lung biopsy, that may be unsafe for such patients. It is also important for clinicians to know who is not infected with this fungus, as the necessary medications are expensive and have potentially toxic side effects.
Draper and Brigham & Women’s Hospital (BWH) are collaborating on a bedside, breath-based diagnostic test that could yield results within minutes, rather than the days or weeks typical of existing measures, without the risks of invasive methods.
“Antifungal medications are very effective against invasive aspergillus, but too often, patients get them too late,” said Tim Postlethwaite, program manager for the breath diagnostic project in Draper’s Biomedical Solutions group.
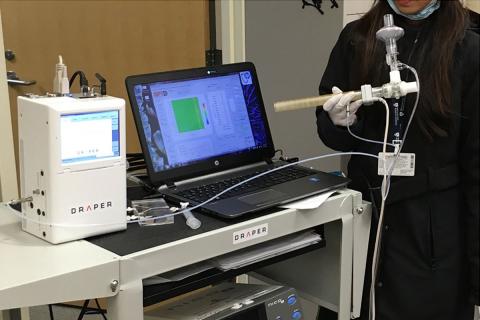
During ongoing clinical studies with a prototype version of the Compact Gas Chromatography – Differential Mobility Spectrometry (GC-DMS) for Breath-Based Diagnostics system, Draper and BWH have demonstrated the ability to correctly diagnose patients with invasive aspergillosis. Draper is working on making the device simpler and more user friendly so that it can be operated by hospital personnel other than certified lab technicians.
“Patients with compromised immune systems are vulnerable to many kinds of lung infections, including fungal and bacterial pneumonia, but current diagnostics for these diseases are very limited,” said Dr. Sophia Koo, a physician in BWH’s Division of Infectious Diseases who is piloting the GC-DMS for Breath-Based Diagnostics in the clinical setting. “Having a device that can rapidly detect and diagnose fungal infection could help us prescribe the right treatment to patients faster and save lives.”
The editors of Clinical Infectious Diseases chose a paper by the Draper/BWH collaborators that discussed earlier work on the project as the “most outstanding clinical study” published in the peer-reviewed journal in 2014.
Draper and BWH are also studying use of this diagnostic capability to distinguish between bacterial and viral pneumonia infection. A presentation on this aspect of the work was selected by a panel of philanthropists, Brigham faculty, and invited experts as one of two winners of a competition for the Brigham Research Institute’s Health and Technology Innovation Fund grants on May 24.
Draper’s diagnostic solution uses the company’s microAnalyzer, a GC-DMS-based device that can detect a variety of compounds in a single sample and is remotely reprogrammable to address emerging concerns beyond aspergillosis. Draper’s microAnalyzer is used today by customers including NASA, which uses it onboard the International Space Station (ISS) to monitor air quality, detect and measure amounts of targeted chemical compounds, and verify the presence of airborne chemicals that could threaten astronaut health and safety.
The GC-DMS system also includes a breath-sampling tube, disposable mouthpiece, and pressure and carbon dioxide sensors that measure whether the patient is providing enough breath to serve as an adequate sample.
The project brings together Draper’s biomedical solutions expertise in developing new technologies and advanced devices with the clinical expertise of BWH’s infectious disease physicians, who provide patient care and consultative services to the BWH community while advancing the hospital’s goals of fostering innovative biomedical research and teaching.
Draper and BWH are currently seeking a transition partner to take the diagnostic device through clinical trials, which could occur within the next two to three years.
Released June 22, 2016