Draper Uses the Body's Self Defense to Find Cancer Therapies
CAMBRIDGE, MA – Cancer causes one of every four deaths in the United States and bears a direct cost to our health care system of close to $100B annually. Over the past several decades, therapeutic approaches toward cancer have developed around surgery, radiation and chemotherapy. And yet, a key challenge remains for biomedical researchers: how to develop tools that accurately predict treatment efficacy against a patient’s specific cancer, thereby avoiding subjecting the patient to a potentially life-threatening trial-and-error process to find the best drug.
Draper engineers, who have developed technologies to treat failure of the liver, kidney, lung and other organs, created a microfluidic system that brings the individual patient into the therapeutic compound discovery process for cancer therapies. By marshaling a patient’s immune system to destroy their cancer—a method known as immuno-oncology—clinicians using Draper’s device can refine and accelerate cancer treatments in ways that extend well beyond the conventional laboratory system, all by tapping into a patient’s own biology.
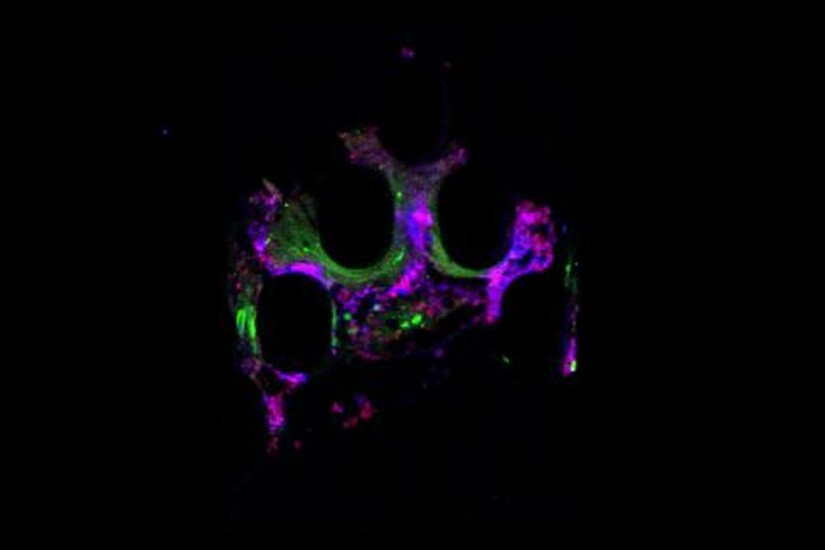
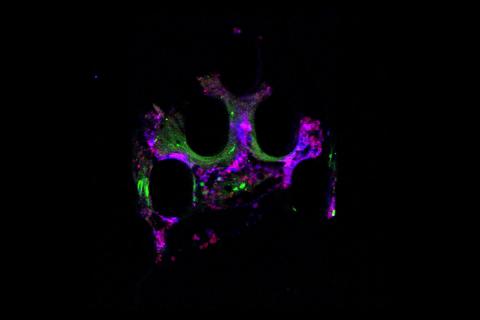
A key feature of Draper’s platform, called the Personalized Predictive Assay for Cancer Treatment (PPACT), is its ability to recapitulate the interaction between a patient’s immune cells and their tumor.
With PPACT, biomedical researchers can create a microenvironment—a test bed of sorts—complete with an engineered vascular-like system containing nutrients and lymphocytes, providing suitable conditions to sustain a 3D fragment of the patient’s biopsied tumor tissue. A precision-controlled microfluidic system delivers various drugs or combinations of drugs along with lymphocytes treated with various compounds, to determine which are most effective at killing the patient’s cancer. The current prototype is a 12-channel device to support parallel testing of multiple tumor fragments and combinations of drugs. If a drug is observed to kill tissues within the PPACT platform, it provides predictive evidence of clinical efficacy against the patient’s cancer.
Draper’s microfluidics PPACT system fits into the growing field of personalized therapeutics and precision medicine, according to Jeff Borenstein, Laboratory Technical Staff at Draper. In tests, Borenstein and his team found that the PPACT system could recapitulate responses seen in studies with mouse models, but within a framework that permits precision control over the tumor microenvironment and real-time monitoring of immune cell function and tumor response.
“The precision and scalability of the microfluidic design enables testing of a large number of therapeutic combinations simultaneously within time frames as short as one week so that patients can start with the right treatment, right away,” Borenstein said.
Because PPACT incorporates circulating immune cells from individual patients in the microfluidic system, it can test the effectiveness of immunotherapy drugs, which unleash the body’s own immune system to fight cancer. Many tumors have developed the ability to locally shut off components of a patient’s immune system, thereby enabling the tumor to grow and thrive unimpeded. With the right immune checkpoint inhibitor, the ability to block the immune response is turned off, and the patient’s T-cells are able to attack the cancer. When immune checkpoint inhibitors work, they are remarkably successful, producing long remissions, as experienced by Jimmy Carter in 2015. There are currently more than 20 immune checkpoint inhibitor drugs on the market, but not every cancer responds to each one, and conventional tools to predict the best one are inadequate.
For companies in need of more-effective cell therapy processing solutions and drug selection options, Draper’s extensive experience and expertise in biology, microfluidics, system integration and subsystem maturity can be applied to designing closed systems; automated, standardized processes; end-to-end solutions; continuous processing; and scalable solutions. These improvements to processes and technologies can help pharmaceutical companies solve the engineering challenges of production to achieve the cost reductions, accelerated results, reduced risk and increased safety that they need to make precision medicine practical.
Released July 25, 2017